Read more about this family's experience in the Factor V Deficiency article.
Both my stepdaughters were born with severe factor V deficiency, an orphan disease with no treatment except fresh frozen plasma (FFP) after a bleed is recognized. So many people with bleeding disorders now can use prophylactic treatment to avoid bleeds. But not my daughters. I’m certain when someone reads about a girl who does not have a therapy to avoid bleeds, they will have not even the faintest clue what her life must be like.
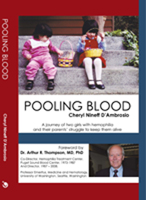
Our hematologist, Arthur Thompson, MD, was the co-director of the Hemophilia Care Program at the Puget Sound Blood Center in Seattle. As he retired, he left us with an inspiring comment: “It’s important to leave something behind.” In an instant, I knew our unique experiences needed to be made available for others to read and hopefully learn from. In March 2010, I published the book Pooling Blood, which shares how our family dealt with some very unusual struggles.
From the time she was an infant, our oldest girl has played the role of teacher—not only to our family, but to doctors and nurses who did not understand what happens to girls with severe bleeding disorders. As the eldest, she went through everything first, including her early bleeds, one of which was inside her head. She was the first to be diagnosed with severe factor V deficiency, and of course the first in our family to deal with a severe bleeding disorder and a menstrual cycle. Sometimes we forget she is developmentally delayed—from a brain bleed as an infant and from subsequent surgery—because she has always shown us the way.
 Clueless New Stepmom
Clueless New Stepmom
Tony was a widower when I met him. On our third date, I met his girls, who were ages 10 and 13 at the time. Tony had mentioned something about the girls having a bleeding disorder, but it didn’t register with me, probably because I didn’t know what a bleeding disorder entailed. One of the early experiences occurred in the middle of the night. We awoke to a thud and screams. Teresa had fallen to the floor. Tony was worried she might have injured her head on the bedroom dresser when she fell, so he took her to the emergency room. Teresa had experienced a cerebral hemorrhage, but the bleeding gradually came under control with FFP infusions.
That event really woke me up. I hadn’t realized so much of Tony’s time was related to caring for the girls and their bleeding disorders, because I was at work at least 10 hours a day. Tony, an architect, had a studio in our home for his job, but he would only work when the girls were not in need of his thoughtful attention.
What happened frequently during the day was that the girls would undergo transfusions at an infusion clinic when they had a bleeding episode. The basic treatment is to infuse two units of FFP for each episode. More units are administered every 24 hours until the bleeding stops. The FFP has the missing clotting factor the girls need. If it’s a simple bleed (like a nose or gum bleed), the bleeding begins to stop soon after the FFP is infused. Serious bleeds, such as in the head or the abdomen, have taken up to 100 units of FFP and one month to subside.
Parental Roles
Tony and I struggled with our desire to make sure the girls didn’t create a situation that would result in a bleed. You might call that being a control freak. Even though I wanted the girls to have a fun life and enjoy things, frequently when I planned something special, it seemed like one of the girls was injured amidst the fun, and I regretted planning the activity.
Also, because I came into their lives during their preteen years, I had difficulty integrating myself as part of the “care team.” Tony and the girls had already established their routines during a bleeding episode. We finally sorted out that during hospitalizations—we would trade shifts. When it was my shift, I took the lead, and when it was his shift, he took the lead. Some hospitalizations would last a week or many weeks, and one parent could not do it alone.
Finding a Way for Safe Activities
When the girls were young, I accompanied them to a camp for families with bleeding disorders called Camp I-VY. One day, the camp staff transformed the mess hall into a carnival for kids of all ages. Both girls entered the pie-eating contest. The oldest entered twice, and her younger sister entered three times. The photos of the girls with whipped cream all over their faces was all the evidence I needed to show how much fun the girls had that week.
Despite the fun of camp, we had to eventually go back to our “real” lives, where it is an exhausting effort trying to lead a reasonably normal life. But I finally “got it.” When I first met Tony, I couldn’t understand why we couldn’t plan trips and have adventures like most families. Now, I understand fully why every activity too far from our hemophilia treatment center is nothing more than a wish for disaster. You might say I have become an official, card-carrying member of the party pooper club.
After our oldest girl was knocked over at a Special Olympics event, I drove her to a local hospital, where I learned they treated only their own military patients. We then took off for Group Health in Bellevue, Washington, about two hours away. I drove her to the ER, and after a brief discussion, the staff ordered FFP. Once again, I shook my head. I should never have taken her so far from her treatment facility, and I shouldn’t have put her at risk around excited kids.
But the damage was done. She had a bleed that traveled from her back into her abdomen, and she needed transfusions throughout the summer. We were lucky she didn’t require surgery. Until things healed, her mobility was severely impaired.
Bleeding episodes have a way of taking so much control over your life. I have heard others say they don’t, but that has not been our experience. When we took a vacation to Kansas City, Missouri, our youngest girl began her first menstrual cycle. Keeping an eye on the situation, I thought we had things under control, but then she fainted. We took her in an ambulance to the hospital, and upon arrival she complained of neck pain, which made no sense to me. “Neck pain is referred pain. She is pooling blood into her abdomen,” the ob/gyn explained. Those two words, “pooling blood,” have never left my mind as the most horrible thought imaginable. I used those words for the title of my book because this situation has occurred to both of my stepdaughters. I am certain it will help prepare the reader for what is to come.
Factor V Deficiency and the Future
Through the years, we have been forever grateful for those who donate blood. Anyone who relies on FFP cannot survive a bleeding episode without the generosity of blood donors. While we begin each bleeding episode with two units of FFP, some bleeds last weeks, requiring many more units.
We’ve had glimmers of hope for potential treatments over the years, but it always gets down to “how many patients need it?” to offset the development, production, marketing and other costs. There are fewer than 200 people in the world known to have factor V deficiency. Being practical, I have nearly given up hope that there will be a treatment product for this very rare bleeding disorder.
I realize everyone wants a happy ending to this story. But we continue to struggle. As long as there is no preventive treatment for factor V deficiency, our lives will continue to be in a time warp, tethered to our local hemophilia treatment center to help bail us out when bleeds occur. Our thoughts and actions revolve around trying to avoid bleeds, negotiating with the medical community to obtain FFP and then transfuse it in a timely manner, and dropping everything we had planned to resolve the bleed once it occurs. Our creativity and strategies to keep the girls alive are what have kept us together as a family and, in some ways, defined our existence as a family unit.

