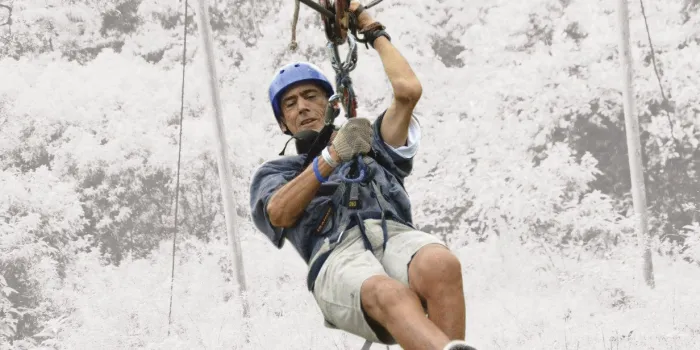
Even though he was born with severe hemophilia A, 59-year-old Ronald Staake of Santa Monica, California, has never let the disorder dictate his life. He has always been active—playing golf, skiing and hiking. “I’m an outdoors person, so I work out to keep my joints as strong as possible, given the bleeds that I’ve had,” he says. Despite his best efforts, however, the joints of both knees and his right hip degraded so much that he had joint replacement surgery on all three: the right knee in 2007, the left knee in 2015 and the hip in 2017.
“It was getting very painful to walk and just do normal everyday things,” Staake says. “The joints were just bone on bone. I had the operations because I wanted to continue participating in all the activities I enjoyed.”
Many people with hemophilia need knee replacements at an earlier age than other types of arthritis patients because bleeds into the joint starting in childhood degrade the cartilage, causing the joint to become arthritic and painful and to lose motion. While all joints are vulnerable, knees, elbows and ankles are the most at risk because they carry the most weight.
“Sometimes it doesn’t take all that long for the arthritis to develop. We see significant joint disease in children, so we know that this can occur fairly rapidly,” says James V. Luck Jr., MD, director of surgical services and rehabilitation at the Orthopaedic Hemophilia Treatment Center in Los Angeles.
“The good news is that number is expected to go down in the future as this new generation that has grown up with better clotting factor replacement (and fewer bleeds) ages,” Luck says. “There are still going to be problems, but not as frequent as before.”
Commonly Asked Questions
Who is the best candidate for knee replacement?
Patients with knee joint arthritis so advanced it’s basically bone against bone, and where the associated pain and lack of motion greatly affect their quality of life. These patients also must be capable of and willing to commit to the rigorous rehabilitation necessary after a knee replacement, says Cindy Bailey, PT, DPT, OCS, SCS, head physical therapist with the Orthopaedic Hemophilia Treatment Center in Los Angeles.
“Patients with a bleeding disorder who have knee replacement surgery need physical therapy more days per week and for a more extended period of time than patients who don’t have a bleeding disorder,” Bailey says. This is mainly because someone with a bleeding disorder is more likely to produce higher levels of connective tissue growth factor (TGF) after surgery, and TGF can make scar tissue form more quickly inside the joint.
Bailey says patients should not have the surgery unless they can commit to the extensive rehabilitation regimen, which includes range of motion and strengthening exercises performed at home.
If you need surgery on both knees, should it be done at one time or staggered?
Orthopedic surgeon James V. Luck Jr., MD, recommends one knee at a time: “The rehab requires a lot of focus from the patients. They need to really concentrate to get good range of motion. Trying to do that with two knees at the same time is too difficult. It’s more than double the trouble.”
Who should do the surgery?
These surgeries are more complex than the usual knee replacement, especially in patients with severe hemophilia. Ideally they should be performed by surgeons with vast experience in the care of bleeding disorders patients, who will work with a team that includes a hematologist with surgery expertise. If that’s not possible, your surgery team should consult with a surgeon and hematologist who are experienced with knee replacements in people with bleeding disorders.
Points to Consider Before Your Knee Operation
Here’s a list of questions you can ask your orthopedic surgeon.
- Does the surgeon have experience in operating on patients with a bleeding disorder?
- Who is on your surgical team? Do they have experience with bleeding disorders?
- Is the team prepared for factor coverage? Most of these surgeries in hemophilia patients are done with continuous infusion of factor.
- Are there plans in place to handle pain? How will the team manage your pain?
- What kind of result can you expect? Keep your hopes realistic. Typically you will regain the range of motion that you went in with.
- Where will you go for physical therapy? How many visits will your insurance plan cover for post-surgical rehabilitation?
- What restrictions in your daily life will you need to adjust to after surgery and for how long?